The IMPACT project seeks to develop sensors that can monitor the strategic biological conditions within tumours in real-time to maximise the effectiveness of radiotherapy, and ultimately chemotherapy, in treating cancer. Such parameters include measurements of acidification (pH) and oxygenation status within areas of tumour, since these are known to adversely influence the success of both radiation and drug treatments. The ultimate target of the clinical/biology strand of the IMPACT project is to translate such sensors into an implantable device that could be used in a clinical radiation setting to optimise treatment outcome. Radiotherapy is applied in the treatment of approximately 65% of cancer cases. This strand of the IMPACT project provides the platform to test the technology of the device.
To enable us to deliver this, the clinical/biology group must ensure that the implantable chip is safe and non-toxic and can be safely delivered into a tumour. To achieve this, this effect of sensor components on cell viability, and the ability of the components to withstand biofouling, have already been assessed in collaboration with the engineering group. Implantation of a ‘mock’ sensor device has been examined using ex vivo tumour tissue, and will be further assessed using human breast tumour xenografts and in an ovine adenocarcinoma model. The ovine model will also be used to monitor the response of tumours to radiation, and to correlate data from the sensors with tumour tissue responses.
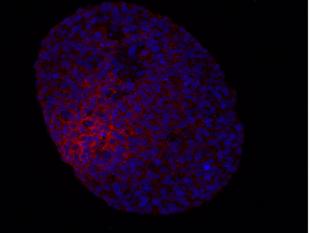
To further investigate the responses of tumour cells and tissues to radiation treatment, we are currently examining the secretory response of irradiated cancer cells in 2D and 3D culture to obtain biomarkers of tumour sensitivity to radiation. These responses will be compared to the secretory response of radiation resistant tumour cells and verified using untreated tumour biopsy samples.
The members of the clinical/biology strand are also involved in the Clinical Translational Group of the IMPACT project which considers the issues involved in the development of the device to the stage of a ‘first-in-man’ study, using information garnered from senior oncologists and scientists.